Your blood tells a story...
Derivations, interactions, correlations
A sophisticated system
The Metabolic Balance programme is based on more than 10,000 calculations, which are applied to your blood results, your body measurements, any conditions you may have and any medications you may be taking.
Some of the recommendations and correlations are obvious, such as increasing iron rich foods if iron levels are low, but others can only be determined by using much more sophisticated algorithms. These have been developed over many years and are based upon extensive research.
Below are just three examples of correlations that are considered when formulating a Metabolic Balance plan. There are hundreds more in the final plan.

1. High triglycerides with normal glucose levels
Research shows that elevated triglycerides with normal glucose levels can acturally indicate underlying factors that are moving a person towards diabetes. Identifying this allows the appropriate measures to be taken (through the plan) so that the progression to diabetes is avoided, and the underlying factors are addressed.
This was highlighted in a study looking at 439 healthy children. Their BMI measurements fluctuated between 18.4 (normal weight) and 40.6 (severely obese). The children were divided into 4 groups depending on their BMI.

All 4 of the children's groups had equally high values for fasting blood sugar, but it was found that the last group were secreting almost 4 times as much insulin. These are fasting values – so we can well imagine that this would be 8 to 10 times higher after a meal. This will be slowly exhausting the pancreas function of these children, eventually leading to Type 2 diabetes..
Triglycerides were found to be twice as high in the obese group compared to those in the normal weight groups. In fact, triglycerides are a very good indicator for obesity and the resulting insulin resistance.
Inflammation markers were also much higher, with C-reactive protein (CRP) up to 33x higher in the severely obese group. CRP is a general marker of inflammation in the body.
These blood markers and correlations are considered when formulating a Metabolic Balance plan.

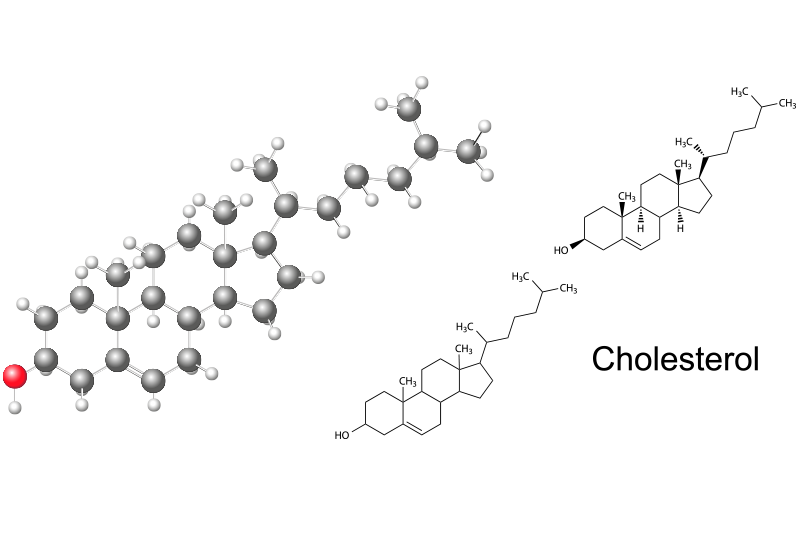
2. Cholesterol formation and metabolism
Most cholesterol circulating in the blood is produced by the body itself, with some coming from the diet. Cholesterol plays many important roles in the body: it is an important component of the cell membranes and also provides the backbone for the production of oestrogen, testosterone and other hormones as well as for bile acids and vitamin D. When your metabolism is functioning correctly, the production and excretion of cholesterol are balanced, but this can easily get out of balance.
Cholesterol also shares a metabolic pathway with Acetyl-CoA, which is produced during the metabolism of fats and proteins ... but especially carbohydrates.
Acetyl-CoA goes on to get converted into HMG-CoA, which is in turn converted into cholesterol and coenzyme Q10. This means that excess carbohydrate consumption can lead to excess production of cholesterol, and high cholesterol levels.
Coenzyme Q10, on the other hand, is used by the mitochondria, the power plants of the cell, for burning carbohydrates and fats in the production of energy.
Cholesterol and CoQ10
If a client is put on statins because of highly-increased cholesterol values, not only is his (or her) own production of cholesterol blocked, but also the production of coenzyme Q10 – and this leads to a slower metabolism in the mitochondira, and lower energy levels.
Reducing foods containing cholesterol (meat, fish, butter, eggs...) will not reduce your total cholesterol. What is required instead is a reduction in the carbohydrate content of a diet. In fact, a reduction from 55% to 40-45% can significantly reduce the total cholesterol in just a few weeks. This is exactly what Metabolic Balance does.

3. Increased uric acid
Uric acid levels can rise in blood due to either an increased intake through food or increased self-production. In high concentrations, uric acid begins to form crystals, which can result in kidney stones or painful gout.
The assumption is that the increased uric acid levels are caused by excessive meat consumption and this has lead to the recommendation to consume low-fat milk, milk products and eggs are as protein sources. Meat and meat products, fish and sausages are only recommended in small quantities, and animal offal, herring, mackerel and smoked sprats, not at all.
However, these recommendations ignore the drivers of the body’s own production of uric acid. In fact, most of the uric acid is produced when there is breakdown of protein from muscle cells, when it is required to make glucose. This process is called gluconeogenesis, which is a normal metabolic process,

Gluconeogenesis causes increased uric acid levels
Gluconeogenesis happens when blood sugar levels in the body cells drop too low so that energy can be made available to the body quickly.
In the case of those who eat too many carbohydrates, the metabolism loses its ability to provide energy efficiently from fats, so instead converts protein into glucose when blood sugars are low, with the consequence that much more uric acid is produced.
So gluconeogenesis is the actual cause of increased uric acid levels, and a lower-carbohydrate and a diet which promotes metabolic flexibility (the ability to use glucose and fats) is the correct way to reduce uric acid levels. A Metabolic Balance plan does both.
Other causes of elevated uric acid levels:
- medicines, such as antihypertensive drugs, acetylsalicylic acid (inhibits uric acid excretion)
- kidney problems – addressing other kidney parameters in the blood count
